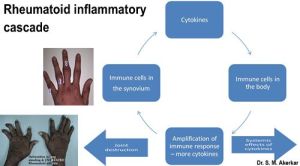
I recently blogged about the ‘drug free remission’ in Rheumatoid Arthritis.
Aggressive treatment with DMARDs, biologics & a targeted approach can help one achieve this.
But, is it really that simple? For the best results, what would one expect from Patients? Positive approach & compliance……
But, why am I thinking about all This?
Last week, I was going through my OPD appointment list. One of the names looked familiar; Mrs. K, but I could not recollect the patient.
A lady in wheel chair, with most of the joints swollen was brought in by 6 of her relatives! She was unable to walk on her own. As I went through her file, history unfolded.
I had seen her some two years back. A lively young lady, a doting mother had consulted me for her joint complaints. She did have rheumatoid arthritis & was started on DMARDs. She was given three DMARDs due to the high disease activity. However, unfortunately she continued to have persistent joint inflammation even after 6 months of therapy.
The inflammation then started interfering with her personal & family life as well. Frequent leaves were ruining her professional reputation, her son was doing badly at school & there were frustration & fights at home.
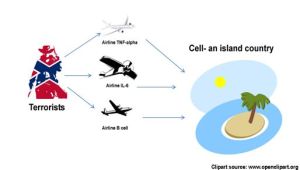
We were slowly moving towards a decision of starting biologics. The entire issue, need of biologics, effects, side effects were discussed. The family was alright with the idea of a more potent drug to control the inflammation, but wanted to wait for some more time. We waited for two months, DMARD doses further optimized; but in vain.
After three months, I discussed the issue again. However, they were scared by a pharmacist relative about the side effects of biologics.
That was the last I saw her then. Now, she started telling me what happened after the last meeting. She & her family were scared of the side effects of biologics, decided to try alternative medicine, stopped all her allopathic medicines. The Result? It was staring at me……
A crucial mistake of stopping all DMARDs at a crucial juncture had done a lot of damage. Her knees were badly damaged & hands were deformed. Time, tide & inflammation does not wait for anyone…..uncontrolled inflammation had inflicted enough of damage already & quite a bit was irreversible.
Suppose you are caught in a similar situation wherein you have to decide regarding a biologic/ new therapy advised by your Doctor, how would you go about?

Decision making made easy for patients
A few points to remember —
1) When you go for a second opinion, if the second consultant confirms the proposed line of treatment, go back to your primary consultant who already knows you & your disease. The second doctor would take some time to understand your arthritis & establish his own treatment strategy.
2) Use the internet, get more information. Be judicious in the choice of sites. You can also use the social media to connect with specialists & other patients to learn from their advice, experience.
3) Never stop the ongoing treatment in the mean time. Never go for the radical option of stopping all the medicines without medical advice.
4) Always know when to put a ‘stop- loss’ order. What is this ‘stop loss order’? It simply means that, you should know when to stop wasting time in taking crucial decisions. Your decision & the plan should not take more than 4- 6 weeks (preferably).
Let us not realize that ‘Time, tide & inflammation does not wait for anyone’ the hard way.